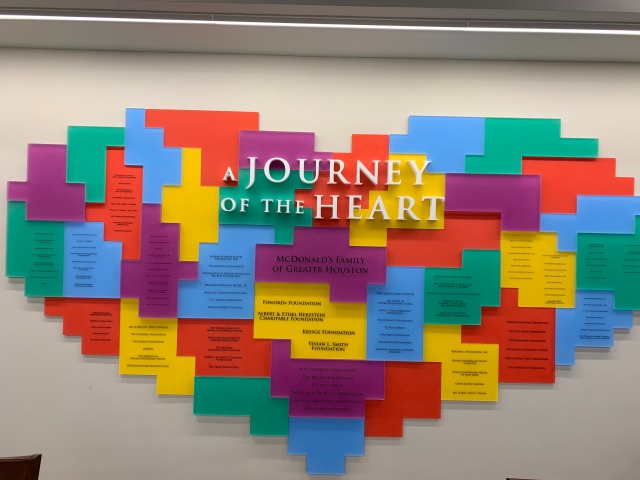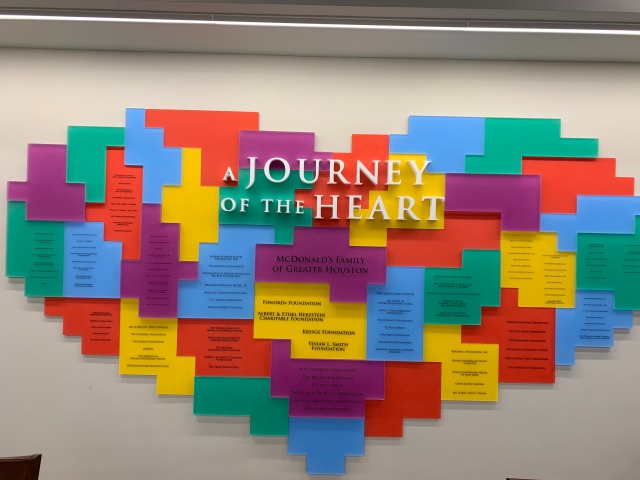
This is in the dining room of the Ronald McDonald House in Houston. We walk by this every single day.
Long post warning…lots happening. Hang in there with me if ya can. (It’s more for me than you…writing helps me organize my thoughts and remember things that I will soon forget!). And I share the nitty gritty details for the heart parents out there so they can understand better what these kids go through and can better prepare themselves for their kid’s future care. I feel it is my obligation to educate and bring awareness to this disease, as I have been given a platform to do so.
Had a productive week of appointments and some much needed down time yesterday. We slept in, ate lunch at the RMDH and then headed out to explore. We are studying Texas battles and some Egyptian history in school. We just learned about the failed battle at the old abandoned Alamo mission in San Antonio and the subsequent battle of San Jacinto where Texas gained it’s Independence from Mexico, and where… I’ll stop there. (REMEMBER THE ALAMO!!)
I tried to get nerdy on you! As my family tells me, you’re dorkness is spilling out and falling on the floor, time to put it back up.
After we visited the San Jacinto monument and museum, which is right on top of the battlefield, we went over and saw the Battleship Texas, a WWI era ship. Super cool! Kaston is a Texan Patriot at heart and really enjoyed the experience (even if he says he didn’t).
Then we headed over to the Museum of Natural Science & History. We only had 30 minutes so we did some speed walking through ancient Egypt…YES! Mummies galore. We definitely will make time to spend a day there during our next trip.
Then spent the evening relaxing at the RMDH with dinner and Kaston chillin in the game room playing video games. They kicked him out at 9:00….he was all wait, what? So he put in a request to keep the game room open later for teenagers 16 and older. They liked the idea…we’ll see.
So what did this week’s tests show? Essentially, no improvement, liver labs slightly worse but not concerning, cardiac stuff about the same. He does have severe liver disease. It’s not ideal, but the good thing is that his liver is still functioning ok and he doesn’t seem to have any side affects that we have identified and there is nothing to treat. We just wait and watch and monitor. We don’t foresee any improvement. As there is really no plan or research on how to improve it. So right now the goal is to slow the progression down as much as possible.
The biggest concern right now is his low heart rate. He runs in the 40s normally. Dropping into the high 20s & 30s during sleep. Of course this is not normal…but what is normal for a Fontan patient? Ha! Nothing. Basically, his natural pacemaker is just not keeping up. And it hasn’t for quite some time, this we have known for years. It’s just getting slower and slower. And for someone as active as Kaston, this could potentially be what’s causing his fatigue. But Dr. Dreyer is more of a structural/disease cardiologist. So he is going to conference with an EP to see if they think the next thing we do should be a pacemaker.
So, an electrophysiologist (EP) is a cardiologist that specializes in the electrical system of the heart. So let’s add yet another doctor to the list.
Which brings us to November. The current plan is to do liver labs and consult with Hepatologist and start evaluating for potential pacemaker with Electrophysiologist. Will probably go ahead and do an echo while we’re there. Might as well, right? Also will see his new Psychologist and the Psychologist that evaluated him when he was 12. They want to reevaluate his neurological status and do a full work up before he turns 18. Dr. Schwartz specializes in cognitive and neurodevelopmental outcomes in survivors of congenital heart disease. They typically do this every 2 years with their Fontan patients. So we will be about 5 years behind come November.
It’s really REALLY hard for us to be putting him through so much all at once. I so much just want to let him be a dang kid. But we are sorta back pedaling and playing catch up with the TCH Fontan program. Dallas just doesn’t have the same proactive approach, so TCH is making sure they have alllllll of their i’s dotted and t’s crossed, especially as he transitions into adult care. And, if there’s SOMETHING we can do to prolong the need for transplant and keep his current heart strong, then that’s what we need to do.
We still want to give his body time to adjust to the Sildenafil. Good thing is that it’s not hurting him, so we will keep on that route for now. Come January, he wants to do a heart cath to check those pressures again. If we see improvement from the Sildenafil, we keep him on it. If no change, we take him off. And liver doc wants another sono w/Elastography and/or another MRE at that time.
If they determine he needs a pacemaker after November appointment, we will schedule that surgery for January as well. The cath and the pacemaker will be 2 different surgeries and the PM will require hospitalization. They will cut him at his sternum, but not bone, just through his skin, to place the leads onto the heart. So it’s still a pretty intense surgery for someone that has his cardiac anatomy. Then the battery part goes up underneath his lower ribs. This is not your standard pacemaker placement and we have to weigh the risks to the benefits. I really have no idea what life with a pacemaker looks like and how all of the moving parts work. So add that to the list of things I need to learn and teach to Kaston so he has a better understanding.
The idea is that if they get his heart rate up, he will have more energy, and the best thing is that it could potentially help his heart function even better. Which in turn could help the liver too.
He feels his heart function is pretty good right now and liver is functioning pretty good as well. Nowhere near needing a transplant at all, which we pretty much knew with the testing in May. As far as time line for when he needs a transplant…of course there’s absolutely no way to know.
He did say that when that time comes, and it will, that they would most definitely do a double transplant. He agreed with Dr. Hertel (liver doc) that it would be way more feasible and a better outcome to get a new liver along with the new heart. Whether you’re transplanting one organ or 2 really doesn’t matter. A new heart working with a new healthy liver is better than working with a diseased and damaged liver. So really, it would be way better to do it that way. I have been under the assumption that we want to keep the liver at all costs, but this actually makes more sense. Plus, there is new technology out of Stanford where they can transplant them at the same exact time. I think it’s called a block harvest? Something like that? Dr. Hertel talks fast and I don’t take notes. I should start recording her consults!
So now we either wait for the heart to fail, or we wait for the liver to fail. Or both together. We could be talking within a year…could be years down the road. We are going for the latter.
So, looks like, for now anyways, we’ll be making our way down here every couple of months for a bit. 😩 So in November we’ll be down here for about 10 days again and then probably a couple of weeks in January if they decide on the pacemaker route. We’re gonna need airline miles if anyone’s got extras they wanna share! 😳
He seems to emotionally be handling everything ok. I guess he’s just used to it by now? He just wants to be home to hang with friends, play video games, shoot guns, ride dirtbikes, not talk about it and just Let It Be.